Rectal prolapse
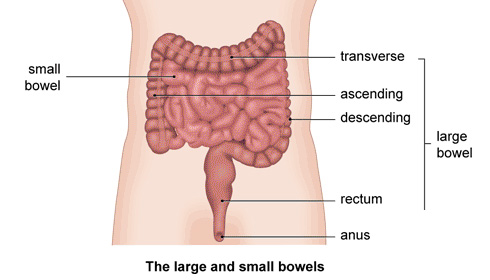
Your rectum is the last part of your digestive system. Food passes through your small bowel (the longer, thinner part of your bowel) and nutrients are absorbed. Food waste then travels through your large bowel where it becomes solid faeces. Your rectum, at the end of your large bowel, is where faeces collect before passing through your anus as a bowel movement.
Your rectum is made up of three layers and includes:
- the rectal wall lining (mucosa)
- a layer of muscle (muscularis propria)
- fatty tissue surrounding the rectum (mesorectum)
Rectal prolapse occurs when the wall of your rectum, or part of its lining, protrudes through your anus. This may happen when you’re having a bowel movement. However, it can also happen when you cough or sneeze, or even when you’re doing everyday activities, such as walking or standing up.
Rectal prolapse mainly affects women – it’s most common in women aged over 50. However, it can happen at any age and also affects men. Young children (usually under three) may also get rectal prolapse and it affects girls and boys equally.
Types of rectal prolapse
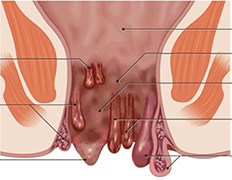
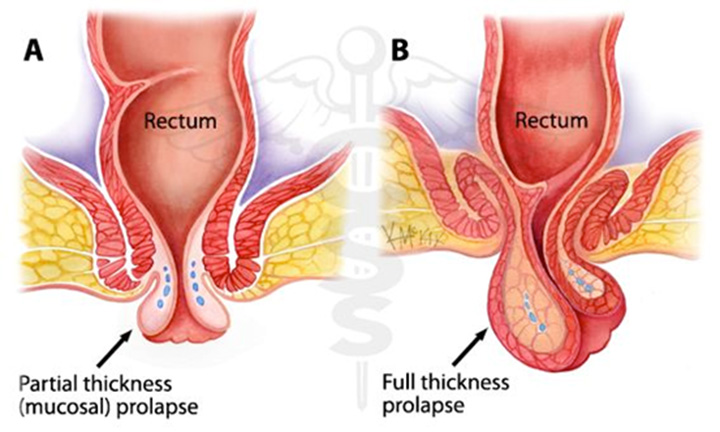
There are three main types of rectal prolapse.
- Full-thickness rectal prolapse is when part of the wall of your rectum (including all three wall layers) protrudes through your anus.
- Mucosal prolapse is when the lining of your rectum protrudes through your anus.
- Occult or internal intussusception rectal prolapse is when your rectum folds in on itself but doesn’t protrude through your anus.
Symptoms of rectal prolapse
 The most obvious symptom of rectal prolapse is a lump or swelling coming out of your anus. Initially you may only have this when you have a bowel movement. However, as the condition develops it may also happen when you cough or stand up. If you have internal intussusception rectal prolapse, there may be no lump or swelling coming through your anus. However, you may feel as though something is still in your rectum after you empty your bowels.
The most obvious symptom of rectal prolapse is a lump or swelling coming out of your anus. Initially you may only have this when you have a bowel movement. However, as the condition develops it may also happen when you cough or stand up. If you have internal intussusception rectal prolapse, there may be no lump or swelling coming through your anus. However, you may feel as though something is still in your rectum after you empty your bowels.
You may find that you’re able to push the lump back in using your fingers. However, it may become difficult and as soon as you push it back in, it may protrude out again. You might not be able to push it back in at all.
If you have rectal prolapse, it can make it difficult for you to control your bowel movements. You may end up soiling your underwear or have a slimy discharge from your rectum. These symptoms can make it difficult for you to maintain good hygiene.
You may have some bleeding from your rectum and discomfort in the area. You may also develop an ulcer on the prolapsed part of your rectum.
Complications of rectal prolapse
Although very rare, part of your rectum can become trapped. This can cut off the blood supply and cause the protruding mass of tissue to die (this is called strangulated prolapse). It can be extremely painful and may cause the prolapsed part of your rectum to swell. If this happens, you must seek urgent medical attention.
Causes of rectal prolapse
The exact reasons why you may develop rectal prolapse aren’t fully understood at present, but it’s often associated with weakened muscles in your pelvis. It’s known to be related to certain conditions that put extra pressure on your abdomen (tummy), such as:
- pregnancy
- constipation and/or straining when you have a bowel movement
- diarrhoea
- conditions that cause you to cough a lot, such as cystic fibrosis, chronic obstructive pulmonary disease (COPD) or whooping cough
Rectal prolapse is also occasionally related to neurological conditions, including:
- multiple sclerosis (MS)
- lumbar disc disease
- an injury to your lower back or pelvis
- spinal tumours
In older women, rectal prolapse can occur at the same time as a prolapsed womb or bladder. This is thought to be due to a general weakness in your pelvic floor muscles. These are the group of muscles that form a supporting sling between your pubic bone and the base of your spine. This weakness in your pelvic floor muscles may be related to previous pregnancy and childbirth.
Diagnosis of rectal prolapse
Your GP will ask about your symptoms and examine you. He or she may need to insert a finger inside your rectum to examine you. Your GP will wear gloves to do this. He or she may also ask you about your medical history.
Your GP may be able to diagnose a rectal prolapse by examining you. He or she may refer you to a doctor who specialises in conditions that affect the bowel for further tests. These may include:
- evacuation proctography –this is a type of X-ray or scan that shows your rectum and anal canal when you’re having a bowel movement
- sigmoidoscopy – this uses a thin tube with a light and camera at the end to allow a doctor to look at the inside of your rectum and bowel
- colonoscopy – this uses a narrow, flexible, tube-like telescopic camera called a colonoscope to allow a doctor to look inside your large bowel
- endoanal ultrasound- this uses a thin ultrasound probe to look at the muscles used for bowel control
You may also need to have other tests to rule out any underlying conditions that may be causing your rectum to prolapse.
Treatment for rectal prolapse
In the early stages of your condition, your doctor may advise you to eat plenty of fruit and vegetables and other foods that contain fibre. He or she may suggest you take bulking laxatives, such as Fybogel, to help you empty your bowels without straining. Your doctor will also advise you to drink enough water.
 In children, rectal prolapse usually gets better without any treatment. Your GP will give you advice on how to get your child into a regular bowel routine. Ensure your child has plenty of fruit and vegetables in their diet, as well as foods that contain fibre. Also ensure your child drinks enough water. Your GP will also advise you on how to push your child’s rectum back into their anus when it prolapses.
In children, rectal prolapse usually gets better without any treatment. Your GP will give you advice on how to get your child into a regular bowel routine. Ensure your child has plenty of fruit and vegetables in their diet, as well as foods that contain fibre. Also ensure your child drinks enough water. Your GP will also advise you on how to push your child’s rectum back into their anus when it prolapses.
Occasionally, your doctor may recommend your child has an injection of a substance called a sclerosant to help destroy the prolapsed tissue or surgery. However, this is only considered if other treatments have not been successful. It will also depend on how old your child is and how serious their condition is.
Surgery
The only way to effectively treat a full-thickness rectal prolapse is to have surgery.
There are different types of surgery, but each type falls into two broad categories. This depends on where your surgeon will make the cut to operate on you. Your surgeon will either make a cut in your abdomen (one cut or a number of smaller cuts), or around the prolapse itself. If around the prolapse, it’s known as perineal surgery.
Your surgeon will advise you on the best type of operation for you. It’s important to remember that the rectal prolapse may come back after you have surgery by either method. The likelihood of a successful operation will depend on the type of surgery you have and your individual circumstances. Ask your surgeon for more information.
Our Expertise in Medical Services
Rana Hospital was started with a dream of providing the best facilities for Piles, Fissures, Fistula and all Anorectal problems.

Mon to Sat:
8:30 AM – 1:30 PM
4:00 PM – 6:30 PM
Mon to Sat:
9:00 AM – 1:30 PM
4:00 PM – 6:30 PM
Make an Appointment
 Accreditation & Awards
Accreditation & Awards
The Hospital organized a free checkup camp for PILES on 24th October 2013 in which 717 patients from all over India were examined. It was followed by one day free operation camp on 27th October 2013. Dr Suri single-handedly performed 391 free surgeries in 8 hours & 45 minutes setting a World Record.